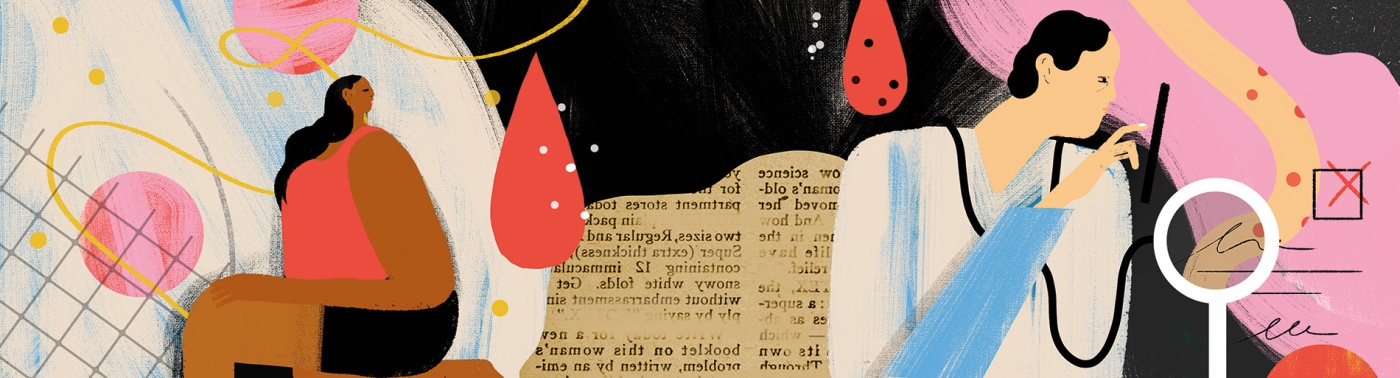
Patients Who Were “Never Prioritized”
Sickle cell, which primarily affects Black people, has been ignored for years. Researchers are coming up with better ways to treat it.
Patrick McGann has a vision for what sickle cell care should look like.
It starts with care throughout a person’s lifespan, from childhood into adulthood. It includes immediate, no-judgment treatment for the pain that’s so often a symptom. Ideally, a center would put all of the providers for people experiencing sickle cell under one roof—from doctors to nurses to social workers.
But for nearly a century, that kind of care has been difficult, if not impossible, to come by for patients with sickle cell disease—a chronic, lifelong condition that affects hemoglobin, the protein that carries oxygen through the body, and is often accompanied by debilitating pain.
“What we’re trying to do here is show what comprehensive sickle cell disease care looks like,” says McGann, a Brown professor of medicine and pediatrics who is the director of the Comprehensive Sickle Cell Center at Lifespan, which treats 300 patients every year. Since arriving at Brown’s Warren Alpert Medical School in 2021, McGann has helped to transform the sickle cell care program by integrating the pediatric and adult-care sickle centers at R.I. Hospital and Hasbro Children’s Hospital.
McGann is also laying the groundwork for a separate Lifespan building to lead the way in comprehensive treatment for the condition.
Taneisha Wilson ’18 ScM, an ER doctor and assistant professor, notes that the vast majority of sickle cell patients are Black and have long faced racism when seeking care. “Our patients just wanted to be treated like humans,” she recalls. “They felt dehumanized not just because they had a chronic disease, but also because they were being racialized.”
A long history of poor care
Lydia Pecker ’03 was first introduced to the history of how race affects health and life outcomes as an undergraduate Africana studies concentrator. Working with history professor Seth Rockman, she wrote an undergraduate thesis on African American communities in antebellum Providence.
Over a decade later, after graduating from medical school and settling into a role treating and studying sickle cell disease at Johns Hopkins University in Baltimore, Pecker was finally able to use her skills in the archives to study the history of sickle cell care at Hopkins.
“I have always had a sense that there’s a strong biomedical story here,” Pecker says. “Sickle cell disease has a past and a future, and its development is intertwined with global geopolitical forces, and struggles to fund research, and the history of my patients… Diseases have context, and especially sickle cell. Time, place, science, history—all matter here.”
The sickle cell mutation first occurred generations ago throughout sub-Saharan Africa and India as a response to malaria. Individuals with the mutation were less likely to get malaria or die from the disease. That means that in many African countries, as many as one in four people have sickle cell trait.
“We need to recognize that these patients have never been prioritized, they are often stigmatized, their care is suboptimal, and we need to proactively address all of these inequalities,” says McGann. “That’s never been done.”
While treating patients in the ER, Wilson, who is Black, has played a central role since 2019 in leading discussions about antiracism and healthy equity training for providers, especially as it relates to sickle cell. She has shared data with other providers about how race-based bias affects quality of care, led discussion groups on racism in healthcare, and helped change how the emergency room at Lifespan treats patients who come in reporting pain from sickle cell.
Pain is a common symptom for patients with sickle cell disease. Some patients describe feeling as though nails or ice were being pushed through their veins. But when people routinely come to the ER seeking help, providers who aren’t aware of the pain associated with the disease sometimes paint them as drug-seeking, which can severely lower the quality of care they’re given.
“That’s why these multidisciplinary discussions with Pat’s team are so important,” says Wilson.
A new era of comprehensive care
When McGann took the job as the director of Lifespan and Brown’s sickle cell care program in 2021, he came in with a mandate to connect the pediatric and adult sickle cell programs at the hospital, creating more continuous care.
Typically, patients come in for routine visits every few months, or more often if they have complications. Forming close relationships with providers is pivotal for treating the disease over the course of a lifetime. But for many, leaving the pediatric sickle cell center at a typical hospital means severing decades-long relationships—often leading to poor outcomes.
In Providence, patients of all ages now come to the same center to receive care and can stay with providers over decades—providers who are now more likely to look like them. McGann has diversified the care team, and more than half now identify as people of color, including some with sickle cell.
“The patients always say, without fail, that they wished people listened to them and treated them seriously and humanely,” observes McGann. “There’s a lot of work to do to try and reduce the racial stigmatization of patients.”